Gynecologic Cancer Awareness Month
What You Need to Know
September is Gynecologic Cancer Awareness Month. Now is a great time to visit the OBGYN. These cancers all involve the female reproductive system, and all women are at risk for them. In fact, The CDC says about 94,000 women are diagnosed with a gynecologic cancer each year. Your risk of getting cancer also increases with age. Since there are so many signs and symptoms, we talked with the Patty Brisben Foundation for Women’s Sexual Health’s Medical Advisory Board to get answers so you know what to look for.
What is Gynecologic Cancer Awareness Month? Why is it important?
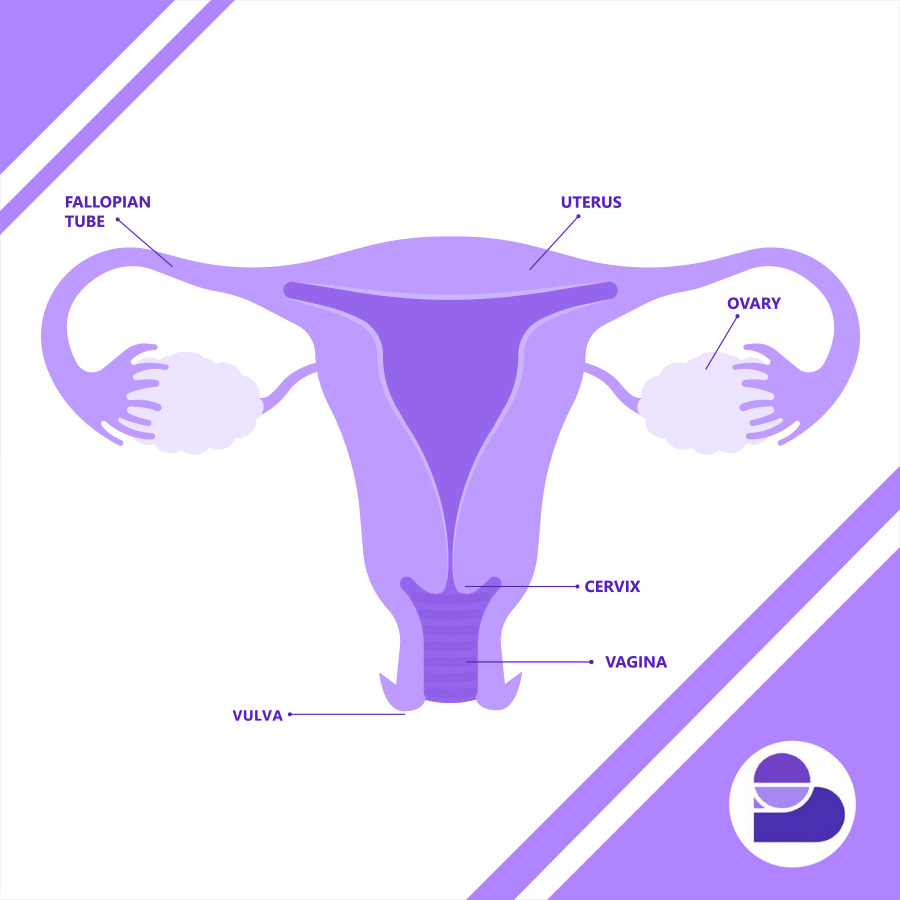
Gynecologic cancers can involve internal organs such as the cervix, uterus, ovary, and fallopian tubes. Additionally, cancers can also occur in the vagina and vulva. Screening for gynecologic cancer is important because cancer is best treated at early stages. We screen for gynecologic cancers through visual inspection of the vulva and vagina, Pap smears of the cervix or vaginal cuff, careful histories, including inquiring about abnormal uterine bleeding (particularly in postmenopausal women), and with biannual pelvic examinations. Cervical cancer and vulvar or vaginal cancers can also be prevented with HPV vaccination prior to exposure to high-risk human papillomaviruses. Furthermore, patients with hereditary breast and ovarian cancer conditions deserve earlier and more frequent screening.
What should we be aware of when it comes to gynecologic cancer?
Common gynecologic cancers include cervical, uterine, and ovarian cancers. The good news is that cervical cancer rates are on the decline due to screening tests (Pap smears and HPV testing) and HPV vaccines. Yay for medicine! If you are overdue for a cervical cancer screening and/or interested in the HPV vaccine, make an appointment to discuss this with your healthcare provider. If cancer prevention isn’t enticing enough for you to get another shot in your arm, the HPV vaccine also protects you from genital warts!
More good news: most uterine cancers are detected early due to vaginal bleeding after menopause. Because they are usually detected early, you usually have a good prognosis. Vaginal bleeding after menopause is NEVER OK, so please see your gynecologist if you have this symptom. Maintaining a healthy weight can help prevent uterine cancer.
Now for the bad news: there is no screening test for ovarian cancer. But, if you are at average risk, there is only a 1% lifetime chance of ovarian cancer. However, if you have a first-degree relative with ovarian cancer, genetic testing should be discussed with your healthcare provider.
What do doctors recommend you do to protect yourself?
The bottom line is annual preventative visits with your healthcare provider are important! If you are overdue for a primary care or OB-GYN visit, schedule it now and encourage your friends to do the same. #selfcare
Are there any resources you recommend?
Start with your primary care healthcare provider and ask about screening guidelines or call your local cancer center.
American College of Obstetricians and Gynecologists
Society of Gynecologic Oncology
Any words of advice?
Do not put your healthcare low on the list of priorities. Make time for your annual gynecological examination, get your mammogram and Pap smear when indicated. Know your inherent risks for certain diseases and get genetic testing if warranted. Be an advocate for your own healthcare.
If you want to spread awareness and share support for those affected by gynecologic cancer, wear a teal ribbon.